Medical errors happen every day, and patients are being harmed in hospitals. Despite years of tracking and reporting outcome-based quality measures, preventable harm remains widespread, prompting the Centers for Medicare & Medicaid Services (CMS) to launch the Patient Safety Structural Measure (PSSM). This measure, released in August 2024, focuses on structural and cultural root causes of harm rather than just retrospective results of quality improvement initiatives.
In our consultancy practice, we’re finding that many hospital leaders, particularly CFOs, CMOs, COOs, and CEOs, are unaware of the new CMS PSSM reporting requirements for the current calendar year, the level of effort it will take to fully implement the required strategies and practices, and the potential impact to future annual Medicare reimbursement payments for noncompliance.
PSSM: What is it, and why does it matter?
CMS hopes to motivate hospital leaders to increase their investment in safety culture and systems through reporting and public transparency. The PSSM regulatory framework directly links reimbursement to the hospital’s structural commitment to patient safety rather than focusing solely on clinical outcome measures, which have been in place for a number of years. The shift to structural, or leading, indicators reflects a proactive approach to preventing harm before it occurs.
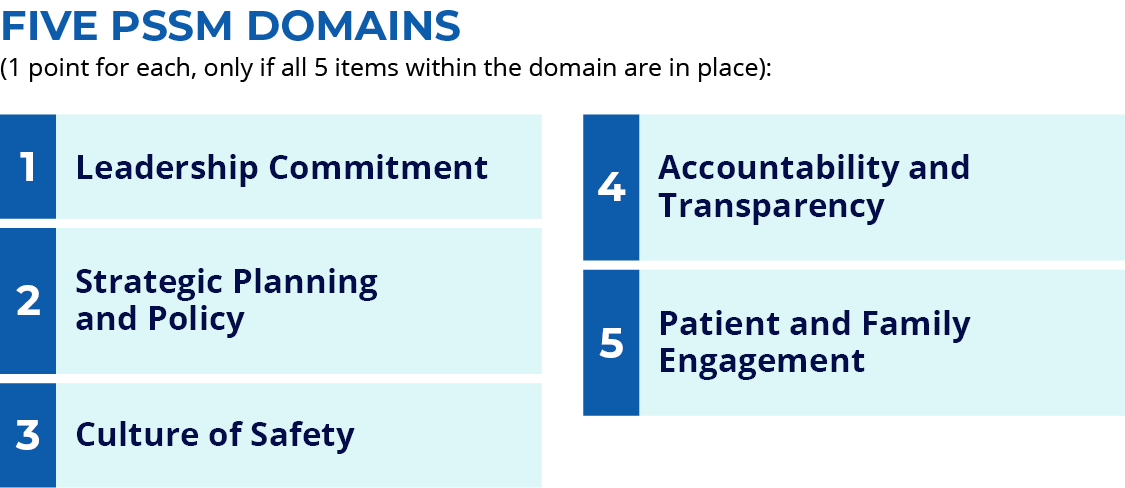
The PSSM evaluates hospitals based on adherence to 25 structural quality and safety elements that, when put in place, facilitate standardization, prevention, and reduction of the clinical variation causing harm. Each PSSM domain (listed below) contains five criteria, and hospitals must attest to meeting all five items to earn the full one point for the domain; partial credit is not given.
Most hospital C-suite leaders are unaware of the scoring details and therefore don’t understand the depth and breadth of change that needs to be implemented for full compliance. Many hospitals completing an early self-assessment against the PSSM attestation statements find they are only scoring a 0, 1, or 2 out of 5 because they don’t have all the infrastructure in place to meet full domain items.
Some requirements are not exceedingly difficult to implement—such as 20 percent of every hospital governing board meeting agenda dedicated to reporting on patient and workforce safety events and initiatives, or completing an annual hospital-wide culture of safety survey using a validated instrument with results reported to the governing board and all staff—but are not always prioritized or fully functional. As the calendar year rolls on, time is running out to get all of the items in place to score the full 5 points.
What’s at stake: reimbursement and reputation
Hospitals face a reduction in the annual Medicare payment for FY 2027 if the PSSM data is not reported for CY 2025. In the current environment of rising costs, Medicaid cuts, and decreasing reimbursement rates, the impact of additional reductions in Medicare payment could substantially impact already shrinking hospital margins. This initial PSSM reporting year is focused on timeliness and compliance with reporting the attestation data; however, in future years, the reimbursement impact will be based on performance and content of the PSSM data itself—potentially even further decreasing CMS payments to those hospitals scoring lower on the 0–5 scale.
In addition, every hospital’s PSSM score (0–5) will be publicly reported on Care Compare starting in fall 2026. Not reporting at all and receiving a score of 0, or reporting and having a score lower than 5, may tarnish a hospital’s reputation. Transparency feeds into patient choice, especially in competitive markets, where negative scores could drive patients elsewhere. Patients are concerned about safety and quality and are increasingly shopping for the right place to receive care—even traveling long distances if they feel it’s necessary. Reputational damage from poor PSSM scores can translate into reduced volume, lower revenue, and diminished community trust.
A roadmap for hospital leaders: operational and culture shift
The PSSM is structured to help hospital leaders identify risks, determine what is not working well, and establish the culture and resources necessary to address root causes of patient harm.
Strong governance is critical. In support of a true culture shift, a C-suite executive should be designated to lead the hospital’s entire patient safety strategy. A single point of accountability at the executive level is essential to build a high-reliability, harm-free care environment by:
- Embedding safety into every facet of hospital operations.
- Maintaining transparency.
- Ensuring alignment between executive leadership and the board.
Board members need to receive regular updates on safety data, prioritize resources aligned with zero-harm goals, and integrate safety into strategic planning, driving patient safety as a top priority from the highest levels of decision-making.
Readiness for PSSM reporting begins with a detailed gap assessment against the 25 required safety elements. This means more than cataloging current practices and checking boxes; it requires verifying that all five required actions in each domain are fully in place and functioning as intended. Once gaps are identified, executive sponsors should be assigned to own each gap, supported by project plans with accountability and timelines to drive progress and avoid fragmented efforts.
A typically overlooked vital step is expanding safety training to include all hospital staff—not just clinicians. Team members such as registrars and administrative staff are often the first to interact with patients and spot potential risks. Comprehensive, ongoing training and competency assessments for all employees is one of the PSSM requirements and is crucial for creating a true culture of safety.
A strong safety culture connects quality and safety efforts to the direct impact on people. Effective leaders see safety not as a compliance task, but as a core foundational value of the organization that impacts people’s lives—including patients, families, clinicians, and other hospital team members. Having the right culture and structural elements in place reduces adverse events, which in turn:
- Cuts avoidable costs.
- Minimizes rework.
- Frees up bed capacity.
- Boosts staff retention.
- Positions hospitals to achieve high-quality outcomes and benefit from value-based payment models.
By embracing an integrated approach, leadership can ensure that safety becomes both a moral imperative as well as a strategic advantage. Taken as a directive for change, the PSSM requirements form a roadmap not only for compliance, but for long-term operational excellence, cultural transformation, and financial sustainability.
Is your hospital ready?
Kim Adelman is a health care executive.



















![Stopping medication requires as much skill as starting it [PODCAST]](https://kevinmd.com/wp-content/uploads/The-Podcast-by-KevinMD-WideScreen-3000-px-4-190x100.jpg)
![Weaponizing food allergies in entertainment endangers lives [PODCAST]](https://kevinmd.com/wp-content/uploads/The-Podcast-by-KevinMD-WideScreen-3000-px-3-190x100.jpg)


![AI censorship threatens the lifeline of caregiver support [PODCAST]](https://kevinmd.com/wp-content/uploads/Design-2-190x100.jpg)
