Medicine demands fast decisions.
Chest pain in triage. A vague complaint from an elderly patient. A scan with subtle shadows.
But the speed that saves lives can also lead to predictable, systematic errors, especially when we trust our gut too much.
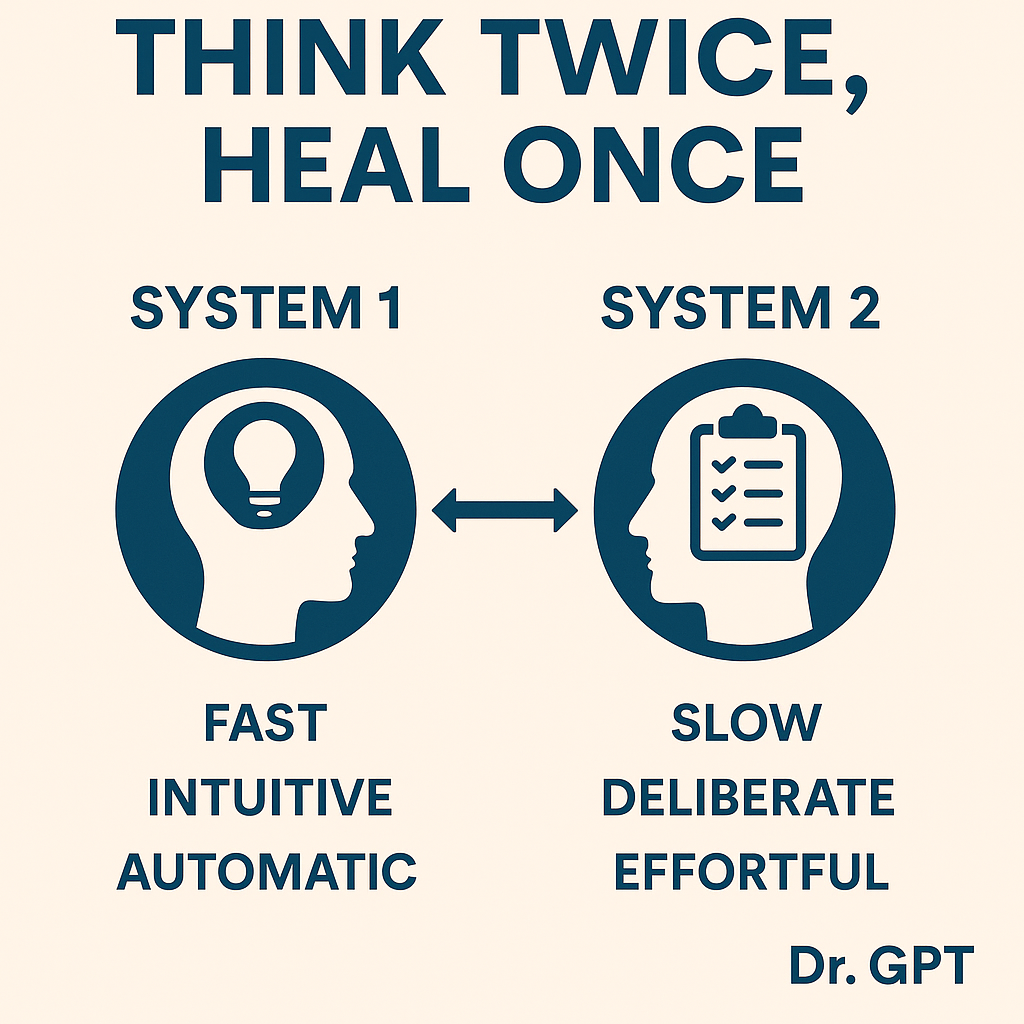
Psychologist Daniel Kahneman taught us that we do not have one mind. We have two.
System 1 is fast, intuitive, and automatic. It makes snap decisions using heuristics and mental shortcuts.
System 2 is slow, deliberate, and analytical. It kicks in for complex reasoning, but only if we activate it.
In medicine, both systems matter. However, most diagnostic errors arise when System 1 makes a quick (wrong) call and System 2 does not intervene.
System 1 biases every clinician faces
Bias is not a character flaw. It is a feature of how human brains save energy. But some of these shortcuts can cause clinical harm:
- Anchoring: The first data point (e.g., a prior note or initial lab) shapes everything that follows, even if it is wrong.
- Confirmation bias: We look for information supporting our hunch, not information that challenges it.
- Premature closure: We stop thinking after the first plausible diagnosis.
- Framing effect: “90 percent survival” feels better than “10 percent mortality,” though both are identical.
Clinical example: A patient returns with abdominal pain. The last visit’s note mentions “muscle strain.” Anchored by that label, the team reassures and discharges. Six hours later, the patient codes from a ruptured AAA.
These are not rare mistakes. They are repeatable patterns unless we build in friction to slow them down.
3 principles for bias-resistant clinical thinking
1. Recognize the limits of intuition. System 1 works well in familiar situations. But novelty breaks it.
Try this:
- Use “red flags” to cue System 2 (e.g., vague symptoms in elderly patients)
- Pause when a case feels “weird” or “off.”
- Build intuition only through feedback-rich learning
Example: An emergency physician’s gut instincts work for trauma cases, but she follows a checklist when elderly patients present with non-specific fatigue or pain.
2. Practice decision hygiene. Kahneman’s recent work emphasizes that bias is not our only problem, and noise (inconsistent judgment) may be worse.
Simple fixes:
- Break complex judgments into parts (e.g., pain score, vitals, history, context)
- Get independent second opinions before group discussion
- Use structured tools to force consideration of alternatives
3. Use debiasing tools like AI
Artificial intelligence is not a replacement for judgment. It is a cognitive assist for your slower brain.
It can:
- Prompt clinicians to revisit differential diagnoses
- Balance recent experiences with historical prevalence data
- Add uncertainty ranges and “Are you sure?” nudges
- Offer opposing hypotheses or highlight overlooked evidence
Example: An AI-enhanced EHR flags subtle early signs of sepsis that a clinician might miss due to “normal” vitals, prompting a timely lactate test and fluids.
Final diagnosis: Slow down when it matters most
Every physician has a fast brain and a slow one. The best clinicians know when to pause and bring System 2 online.
Before your next big decision, ask:
- Am I anchoring to early data?
- Have I challenged my first impression?
- Would a colleague, checklist, or AI offer a different perspective?
Better decisions do not always take longer. But they always take intention.
Harvey Castro is a physician, health care consultant, and serial entrepreneur with extensive experience in the health care industry. He can be reached on his website, harveycastromd.info, Twitter @HarveycastroMD, Facebook, Instagram, and YouTube. He is the author of Bing Copilot and Other LLM: Revolutionizing Healthcare With AI, Solving Infamous Cases with Artificial Intelligence, The AI-Driven Entrepreneur: Unlocking Entrepreneurial Success with Artificial Intelligence Strategies and Insights, ChatGPT and Healthcare: The Key To The New Future of Medicine, ChatGPT and Healthcare: Unlocking The Potential Of Patient Empowerment, Revolutionize Your Health and Fitness with ChatGPT’s Modern Weight Loss Hacks, Success Reinvention, and Apple Vision Healthcare Pioneers: A Community for Professionals & Patients.





















![AI censorship threatens the lifeline of caregiver support [PODCAST]](https://kevinmd.com/wp-content/uploads/Design-2-190x100.jpg)
