Applied Behavior Analysis (ABA) has become the default therapy for autism in the U.S., not because it’s the most effective, but because it’s the most entrenched. Mandated by insurers, funded by Medicaid, and marketed as “medically necessary,” ABA now consumes hundreds of millions of dollars annually. But here’s the truth: ABA is unproven, ethically fraught, and fiscally unsustainable.
As a developmental-behavioral pediatrician and lead investigator for the NIH-funded RUPP trials, I helped finalize the only scientifically validated treatment for the most burdensome manifestations of autism: severe irritability, aggression, and self-injury. That treatment was not ABA. It was risperidone. Later, aripiprazole joined it. Both are FDA-approved. Both were rigorously tested. Both work.
ABA, by contrast, has never passed that bar.
The evidence gap
A 2014 article in Pediatrics titled “Screams, Slaps, and Love: The Strange Birth of Applied Behavior Analysis” exposed ABA’s origins in aversive conditioning, including electric shocks and forced compliance. The authors, Bowman and Baker, documented how autistic children were treated as “not people in the psychological sense,” quoting Lovaas directly. This isn’t ancient history; it’s the foundation of a therapy still widely funded today.
A 2023 article in Frontiers in Psychology built on this indictment. Instead, the authors (Pantazakos and Vanaken) called for a shift toward phenomenological care that honors autistic lived experience. Their work aligns with the neurodiversity movement and validates what autistic adults have long said: ABA is traumatic, coercive, and dehumanizing.
The RUPP legacy
In contrast, the RUPP Autism Network produced eight peer-reviewed studies that shaped the clinical landscape. Our 2002 trial, published in The New England Journal of Medicine, demonstrated that 75.5 percent of children treated with risperidone showed clinically significant improvement in severe behaviors, compared to just 11.5 percent in the placebo group. These results were defined by validated scales: a ≥25 percent reduction in the Aberrant Behavior Checklist-Irritability subscale and a rating of “much improved” or “very much improved” on the Clinical Global Impressions-Improvement scale.
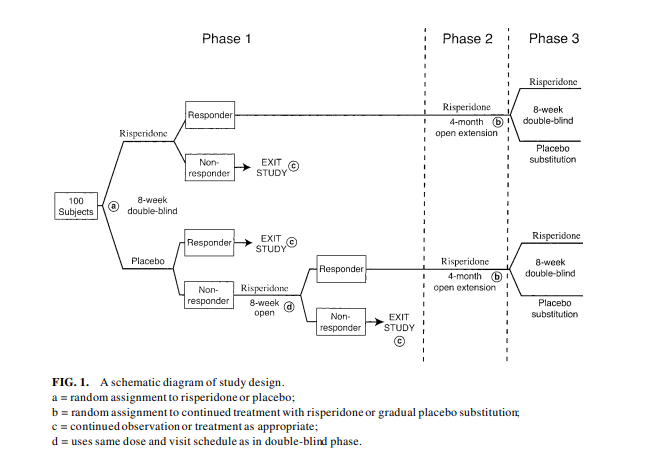
Figure 1. Percentage of children rated “much improved” or “very much improved” on the Clinical Global Impressions–Improvement Scale over an eight-week randomized trial.
- Risperidone group: 75.5 percent response by week 8
- Placebo group: 11.5 percent response
RUPP 2 expanded this work by integrating structured parent training. Published in the Journal of Child and Adolescent Psychopharmacology, the study showed that combining risperidone with caregiver support improved adaptive behavior and reduced parental stress. The “customer approach” emphasized caregiver priorities over rigid behavioral metrics, an ethical and clinical pivot away from ABA’s compliance model.
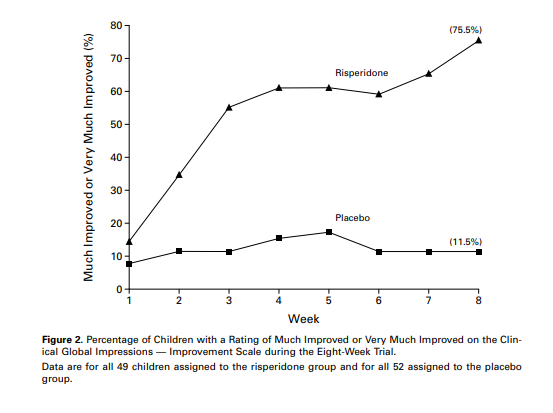
Figure 2. CONSORT-style methodology diagram showing randomized assignment, inclusion criteria, and outcome measures for the RUPP risperidone trial.
The financial toll
In state after state, Medicaid budgets are strained by high-intensity ABA programs that deliver questionable outcomes. In Florida alone, ABA billing has ballooned into the hundreds of millions annually, often with minimal oversight. Families are promised transformation; what they receive is compliance training.
Idaho recently pivoted. The new CHIS model redirects funding toward care coordination, parent support, and trauma-informed services. It’s not just more humane; it’s more cost-effective. Other states must follow.
The ethical reckoning
Autistic adults have spoken. Many describe ABA as traumatic, coercive, and dehumanizing. They’re not rejecting therapy; they’re demanding dignity. As clinicians, we must listen. As policymakers, we must act.
ABA’s defenders claim it has evolved. But the core remains unchanged: behavior modification through external control. That’s not therapy. That’s conditioning.
The path forward
We need to:
- Reclassify ABA as experimental unless proven otherwise.
- Fund therapies with demonstrated efficacy (like risperidone and aripiprazole) for severe behaviors.
- Invest in communication supports, family training, and neurodiversity-affirming care.
This isn’t about ideology. It’s about evidence. It’s about ethics. It’s about ending a costly delusion and funding what actually works.
Ronald L. Lindsay is a retired developmental-behavioral pediatrician whose career spanned military service, academic leadership, and public health reform. His professional trajectory, detailed on LinkedIn, reflects a lifelong commitment to advancing neurodevelopmental science and equitable systems of care.
Dr. Lindsay’s research has appeared in leading journals, including The New England Journal of Medicine, The American Journal of Psychiatry, Archives of General Psychiatry, The Journal of Child and Adolescent Psychopharmacology, and Clinical Pediatrics. His NIH-funded work with the Research Units on Pediatric Psychopharmacology (RUPP) Network helped define evidence-based approaches to autism and related developmental disorders.
As medical director of the Nisonger Center at The Ohio State University, he led the Leadership Education in Neurodevelopmental and Related Disabilities (LEND) Program, training future leaders in interdisciplinary care. His Ohio Rural DBP Clinic Initiative earned national recognition for expanding access in underserved counties, and at Madigan Army Medical Center, he founded Joint Base Lewis-McChord (JBLM) CARES, a $10 million autism resource center for military families.
Dr. Lindsay’s scholarship, profiled on ResearchGate and Doximity, extends across seventeen peer-reviewed articles, eleven book chapters, and forty-five invited lectures, as well as contributions to major academic publishers such as Oxford University Press and McGraw-Hill. His memoir-in-progress, The Quiet Architect, threads testimony, resistance, and civic duty into a reckoning with systems retreat.


















![AI censorship threatens the lifeline of caregiver support [PODCAST]](https://kevinmd.com/wp-content/uploads/Design-2-190x100.jpg)

