I’ve been an X-ray and CT technologist for almost ten years, and I’ve always taken pride in my work. But nothing could have prepared me—or any of us—for what the COVID-19 pandemic brought. It wasn’t just the virus itself; it was the way it exposed the cracks in our health care system, the way it pushed us all to our limits, and the way it changed how we saw our work, our patients, and each other. I want to share some of my story, not just as a technologist, but as someone who stood alongside my colleagues in the trenches, trying to keep up with an endless wave of patients (both COVID and non-COVID) who needed us more than ever.
The early days: Fear and uncertainty
When COVID-19 first hit, everything changed overnight. The hospital felt like a war zone. Patients were pouring in, and we were scrambling to keep up. I remember the first time I scanned a COVID-19 patient—my hands were shaking as I adjusted the machine, trying to focus on the image while my mind raced with questions. What if I got sick? What if I brought it home to my family? But there was no time to dwell on those fears. The patients needed us, and we had to be there for them.
The images I saw during those early months still haunt me. Lungs that should have been clear and healthy were filled with the telltale “ground-glass opacities” of COVID-19 pneumonia. It was unique, it was unusual, and it attacked everywhere in the body. It was devastating to see how quickly the virus could take hold, especially in patients who seemed healthy just days before. And the hardest part was knowing that many of them were alone, isolated from their families, relying on us not just for medical care but for comfort and reassurance.
The struggle to keep up
As the pandemic dragged on, the sheer volume of patients became overwhelming. It wasn’t just COVID-19 cases—it was everything. People who had put off routine care during the early months of the pandemic were now coming in with advanced illnesses. Heart attacks, strokes, cancers that had gone undetected for too long. The waiting rooms were packed, the schedules were overbooked, and we were all running on fumes.
I’ll never forget the look on my colleagues’ faces as we tried to keep up. Nurses, doctors, fellow technologists—we were all exhausted, physically and emotionally. I saw people breaking down in the break room, crying from the stress of it all. I saw coworkers working double shifts, skipping meals, and sacrificing their own health to be there for their patients. And I saw some of the best, most dedicated professionals I’ve ever known leave the field altogether because they just couldn’t take it anymore. Losing them was like losing a piece of our team’s soul. These people were irreplaceable—their wisdom, their dedication—we needed them, and the system failed them. The communities are worse off without them.
The human side of it all
What sticks with me the most, though, are the people—the patients and the families. I remember one elderly man who came in for a CT scan. He was so scared, and all he wanted was to hold his wife’s hand. But she wasn’t allowed in the room because of visitor restrictions. So I held his hand instead, trying to reassure him as I positioned him for the scan. He thanked me afterward, and I had to fight back tears because I knew it wasn’t enough. It wasn’t the same as having his family there. How could it be? And many fellow professionals were too busy and exhausted to provide the level of comfort these people needed—we were stretched way further than usual.
And then there were the families themselves, waiting anxiously for news. I’d see them in the hallways, their faces masked but their fear unmistakable. Sometimes, I’d overhear them talking to doctors, trying to understand what was happening to their loved ones. Other times, I’d see them saying goodbye over video calls, unable to be there in person. Those moments broke my heart in a way I can’t even put into words.
A system under strain
The pandemic didn’t just test us as individuals—it tested the entire health care system. And in so many ways, the system failed. We didn’t have enough staff, enough equipment, or enough time to give every patient the care they deserved. I saw people waiting hours, even days, for scans that should have been done immediately. I saw patients with treatable conditions getting worse because they couldn’t access care in time. And I saw my colleagues—good, caring people—burn out and walk away because they couldn’t keep fighting a system that felt like it was working against them.
It’s hard not to feel angry about it. We’re supposed to be a safety net, a place where people can turn when they’re sick or scared. But the pandemic showed just how fragile that net really is. And now, as we try to pick up the pieces, I worry about what happens next. Will we learn from this? Will we invest in our health care system, in our workers, in our patients? Or will we go back to the way things were, pretending everything’s fine until the next crisis hits?
A call for change
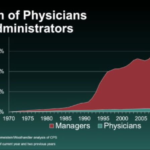
I don’t have all the answers, but I know this: We can’t keep going like this. We need more support for health care workers—better pay, better staffing, better mental health resources. We need to prioritize access to care for everyone, not just those who can afford it. And we need to remember the lessons of this pandemic—not just the pain and the loss, but the resilience and the humanity that got us through it. Patient volumes have only gotten worse since the COVID-19 pandemic, and data trends suggest we will continue to see an exponential increase in people needing care, peaking in 2040.
To my fellow health care workers: Thank you. Thank you for showing up, even when it felt impossible. Thank you for caring, even when it hurt. And to everyone else: Please don’t forget what we’ve been through. Advocate for change. Support your local hospitals and clinics. And remember that behind every mask, every scan, every diagnosis, there’s a person—a patient, a family, a health care worker—just trying to make it through.
This is my story, but it’s also the story of so many others. I share it not for sympathy, but in the hope that it will inspire action. Because if we don’t learn from this, if we don’t do better, then what was it all for?
Kyle Wells is a radiologic technologist.


















![Heat therapy activates proteins that repair cells and protect the heart [PODCAST]](https://kevinmd.com/wp-content/uploads/Design-4-190x100.jpg)

