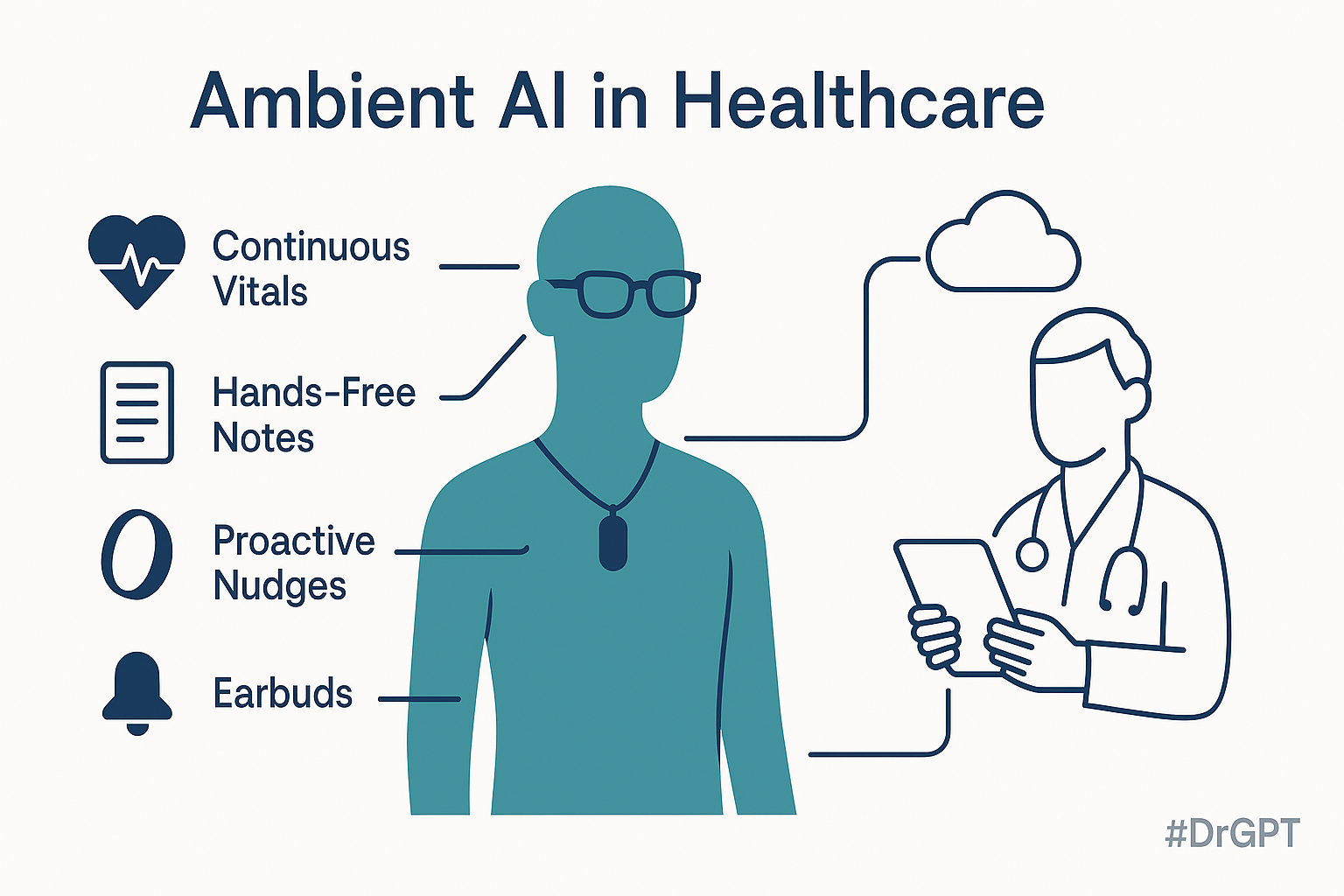
A quiet revolution is taking place in health care technology. AI is shedding its screen-bound constraints and stepping into forms that blend seamlessly into our lives—rings, glasses, pendants, earbuds. These “ambient” devices collect real-time insights from sound, motion, and physiology, surfacing only when needed. For clinicians, this shift means more than convenience: It reimagines how we gather data at the bedside and how patients manage their health between visits.
From step counters to continuous vital signs
First-generation wearables tracked steps and little else. Today’s devices—bright rings, sensor-packed pendants—monitor heart rate variability, oxygen saturation, skin temperature, stress responses, and even sleep-stage micro-movements with increasing accuracy.
Many startups are submitting clinical validation packages to regulators, moving from “wellness” into truly medical territory. Imagine an emergency physician triaging a patient not just by symptoms but with a week’s worth of resting pulse trends or overnight oxygen dips already in hand. That’s ambient AI offering clinical value before a single word is spoken.
Hands-free memory: AI that listens so you can focus
Wearable voice recorders—small enough to clip to a collar or ID badge—can now transcribe conversations on-device and generate structured summaries. For clinicians, that might mean capturing medication changes or discharge plans without the laptop barrier. For patients, it transforms a routine follow-up into a searchable health log. No more misremembered instructions about whether it’s “two tablets twice daily” or “one tablet every twelve hours.”
Design that disappears: Why these tools finally look like jewelry
Adoption hinges on comfort and aesthetics. Smart rings pass for wedding bands. AI glasses resemble classic frames. ID-style pendants blend with scrubs. This design discretion matters: The less intimidating the tech, the more willing patients and clinicians are to use it. The early demise of head-mounted displays taught us that form factor can be just as critical as function.
Startups, crowdfunding, and the open-source Cambrian explosion
Many of these devices launch not through traditional channels but via crowdfunding. These campaigns test demand, fund production, and recruit real-world testers. At the same time, some projects are open-sourcing their hardware and code, allowing a global community of developers to iterate quickly.
Instead of aiming to be all-purpose smartphones, these devices focus on narrow, high-value use cases—like brain-sensing sleep buds or context-aware dictation tools. In the startup world, lean specialization is beating broad ambition.
The promise—and risk—of proactive AI
Ambient AI doesn’t just wait for prompts—it anticipates needs. A headset might whisper, “Repeat the last BP reading,” as you dictate notes. A ring might nudge a hypertensive patient to stand after prolonged inactivity.
But proactivity cuts both ways. Poorly tuned algorithms risk interrupting at inopportune moments or misleading context. The future depends as much on smart filtering as it does on intelligent sensing.
When innovation overreaches: lessons from early failures
Some ambient devices have flamed out quickly. A recent high-profile example was shut down months after its launch, with users citing heat issues, confusing gestures, and unclear benefits compared to existing smartphones. The takeaway? New AI hardware must either integrate seamlessly as an accessory or outperform the phone it aims to replace.
Clinical potential—and ethical responsibilities
Real-world use cases:
- Emergency triage with wearable data arriving before the patient speaks.
- Longitudinal vitals from rings or buds offer more context than a five-minute consult.
- Ambient documentation that restores eye contact and cuts charting time.
- Patient empowerment through AI-curated visit summaries that reduce errors and improve adherence.
But with each opportunity comes a responsibility:
- Data privacy: Devices must encrypt data both at rest and in transit, allowing patients to exercise proper control over data deletion.
- Algorithmic fairness: AI trained on narrow populations may miss early signs in underrepresented groups.
- Regulatory rigor: Wearables guiding diagnosis must meet the same standards as traditional medical devices.
What comes next: a future quietly augmented
In the coming years, ambient AI will continue to blur the line between consumer gadgets and clinical tools. Miniaturized sensors, edge computing, and large language models will make technology invisible—while making human capability more visible.
If we get this right, a future patient might casually say, “My ring caught the arrhythmia before I felt it,” as an ER doc notes, “The summary in my ear halved my charting time.” That’s ambient AI at its best: quiet, constant, and in service of better care.
Let’s guide these technologies not just toward what’s possible—but toward what’s equitable, ethical, and clinically transformative.
Harvey Castro is a physician, health care consultant, and serial entrepreneur with extensive experience in the health care industry. He can be reached on his website, harveycastromd.info, Twitter @HarveycastroMD, Facebook, Instagram, and YouTube. He is the author of Bing Copilot and Other LLM: Revolutionizing Healthcare With AI, Solving Infamous Cases with Artificial Intelligence, The AI-Driven Entrepreneur: Unlocking Entrepreneurial Success with Artificial Intelligence Strategies and Insights, ChatGPT and Healthcare: The Key To The New Future of Medicine, ChatGPT and Healthcare: Unlocking The Potential Of Patient Empowerment, Revolutionize Your Health and Fitness with ChatGPT’s Modern Weight Loss Hacks, Success Reinvention, and Apple Vision Healthcare Pioneers: A Community for Professionals & Patients.





















![AI censorship threatens the lifeline of caregiver support [PODCAST]](https://kevinmd.com/wp-content/uploads/Design-2-190x100.jpg)
