The real limitation of clinical AI isn’t the model; it’s the context.
AI can draft notes, flag interactions, and read scans. However, when it comes to understanding the patient in front of you, it’s still a matter of working in the dark.
It doesn’t know the blood pressure you entered three minutes ago.
It can’t find the beta-lactam allergy buried in yesterday’s note.
It misses the serum creatinine result that just came in from the lab.
The issue isn’t the algorithm; it’s access to real-time clinical context. That’s the gap the model context protocol (MCP) was designed to close.
MCP enables AI tools to operate securely, transparently, and in a manner that preserves compliance within clinical systems. It’s not just another standard. It’s the infrastructure we’ve been waiting for.
What is the model context protocol (MCP)?
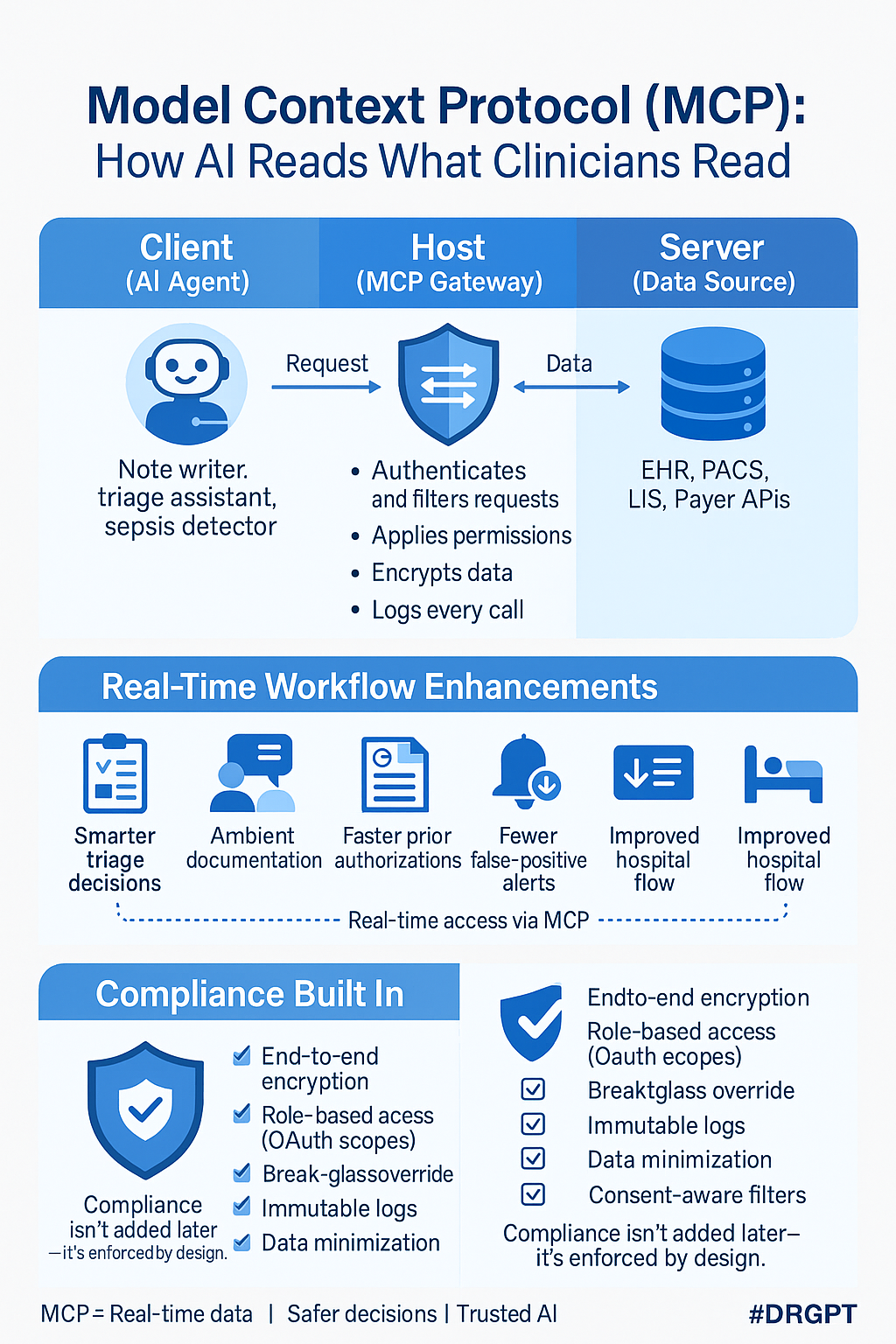
MCP is a lightweight JSON-RPC specification released in late 2024. It provides a standardized way for AI agents to interact with clinical data systems. MCP defines three core roles:
- The AI agent
- The host that mediates data access
- The clinical data sources
In this structure, the AI doesn’t need to know which EHR you use or where the data lives. It simply requests what it needs. The host layer handles translation, applies access controls, encrypts communication, and maintains an audit log of every call.
There is no custom integration. There are no hidden data flows, just clean, controlled access.
Five ways MCP enhances clinical workflow
Informed triage from the start: With MCP, triage assistants can pull the allergy list, med history, and last admission note before the patient is seen. This enables the AI to suggest appropriate triage levels, necessary labs, or infection control precautions. The result: nurses spend less time searching for clinical histories, and physicians receive more structured and relevant handoffs.
Documentation during the encounter: Ambient AI can capture patient-clinician dialogue, retrieve today’s lab results via the MCP, and generate a structured SOAP note in real time. Physicians review and sign. Early pilots show a 40 percent reduction in after-hours documentation.
Streamlined prior authorization: Beginning in 2026, payers will be required to accept FHIR-based prior authorization packets. An MCP-integrated agent can compile relevant ICD-10 codes, imaging reports, and policy language, submit the request electronically, and track its status. This replaces hours spent on phone calls and faxes with a streamlined digital workflow.
More reliable clinical alerts: Most early-warning systems suffer from high false-positive rates because they rely on limited data inputs. With MCP, AI tools can access labs, medications, vasopressors, and vitals. This expanded context leads to higher specificity and sensitivity. Each alert can also include a breakdown of the exact data that triggered it, supporting faster clinical validation.
Optimized hospital flow: Command-center AI systems can use MCP to access census data, staffing information, and discharge barriers. This enables real-time visibility into the following:
- Beds that are likely to become available
- Tests delaying discharge
- Operating room bottlenecks before they occur
Its predictive capacity is grounded in operational reality.
Designed for compliance from the ground up
MCP was architected to meet the strictest privacy and security standards. Built-in safeguards include:
- End-to-end encryption using TLS 1.3
- OAuth 2.0 scopes mapped to specific clinical roles
- Break-glass overrides with automated tagging
- Immutable logs of all data requests and responses
- Data minimization—only what is necessary is accessed
- Consent filtering following state and federal laws
Security and compliance teams gain a central command layer to monitor and control all AI interactions.
What is HMCP?
The health care model context protocol (HMCP) is an industry-specific profile of the model context protocol (MCP) tailored for clinical environments. It provides:
- Alignment with national standards like FHIR U.S. Core
- Terminology normalization across SNOMED, LOINC, and RxNorm
- Risk scoring to block unsafe or out-of-scope requests in real time
- Specialty plug-ins (e.g., DICOM for radiology, VCF parsing for genomics)
Hospitals using HMCP report integration cycles are measured in days, not months.
How to deploy MCP in practice
MCP implementation doesn’t require a complete system overhaul. Early adopters are taking a phased approach:
- Start with a low-risk use case, such as note generation or lab summarization
- Apply “least privilege” access to ensure each AI agent sees only the data it needs
- Introduce audit transparency to give staff visibility into what the AI accessed
- Measure impact: track effects on documentation time, alert quality, LOS, and safety metrics
- Expand to additional use cases: triage, prior auth, discharge management
Governance remains simple because every call, scope, and override is already logged and auditable.
What to expect by 2030
Over the next five years, MCP will become a foundational requirement for clinical AI systems. We are likely to see:
- Documentation assistants who draft notes live in the exam room
- Oncology decision support that synthesizes genomics, trials, and outcomes
- Hospital-at-home models that stream vitals to AI monitors for proactive care
- Global health surveillance that queries de-identified data without violating privacy
All of these depend on the same core principle: AI must access clinical data under the same guardrails that clinicians use.
The bottom line
MCP is not just another tech framework. It is the infrastructure that finally makes real-time, context-aware clinical AI viable.
Physicians gain back time.
Patients receive safer, more coordinated care.
Administrators maintain audit-ready compliance across all AI activity.
If your next AI pilot doesn’t support MCP, the most crucial question is: Why not?
Harvey Castro is a physician, health care consultant, and serial entrepreneur with extensive experience in the health care industry. He can be reached on his website, harveycastromd.info, Twitter @HarveycastroMD, Facebook, Instagram, and YouTube. He is the author of Bing Copilot and Other LLM: Revolutionizing Healthcare With AI, Solving Infamous Cases with Artificial Intelligence, The AI-Driven Entrepreneur: Unlocking Entrepreneurial Success with Artificial Intelligence Strategies and Insights, ChatGPT and Healthcare: The Key To The New Future of Medicine, ChatGPT and Healthcare: Unlocking The Potential Of Patient Empowerment, Revolutionize Your Health and Fitness with ChatGPT’s Modern Weight Loss Hacks, Success Reinvention, and Apple Vision Healthcare Pioneers: A Community for Professionals & Patients.




















![AI censorship threatens the lifeline of caregiver support [PODCAST]](https://kevinmd.com/wp-content/uploads/Design-2-190x100.jpg)
