I once promised myself confidently, and with the full arrogance of a seasoned attending, that I would never sleep another night in a hospital. I’d done my time. I’d earned my daylight. But life has a way of calling your bluff. A few years later, everything had shifted. I was divorced. My kids were older and more independent. My clinical career had settled into something comfortable, but predictable. I found myself craving a challenge and something to pull me out of the mid-career doldrums.
At the same time, the work I was doing with the largest community-powered salary-sharing platform in medicine was growing into something bigger than I had expected. To build it into the kind of platform that could actually shift power back toward clinicians, I needed time, real, uninterrupted time. I didn’t want to leave medicine, so the only way to create that space was to flip my life upside down and take a night-float position, meaning I work nights for a week, with every other week entirely off. I knew that this schedule wouldn’t be easy, but I failed to anticipate all the ways it would be hard.
When night work actually pays off
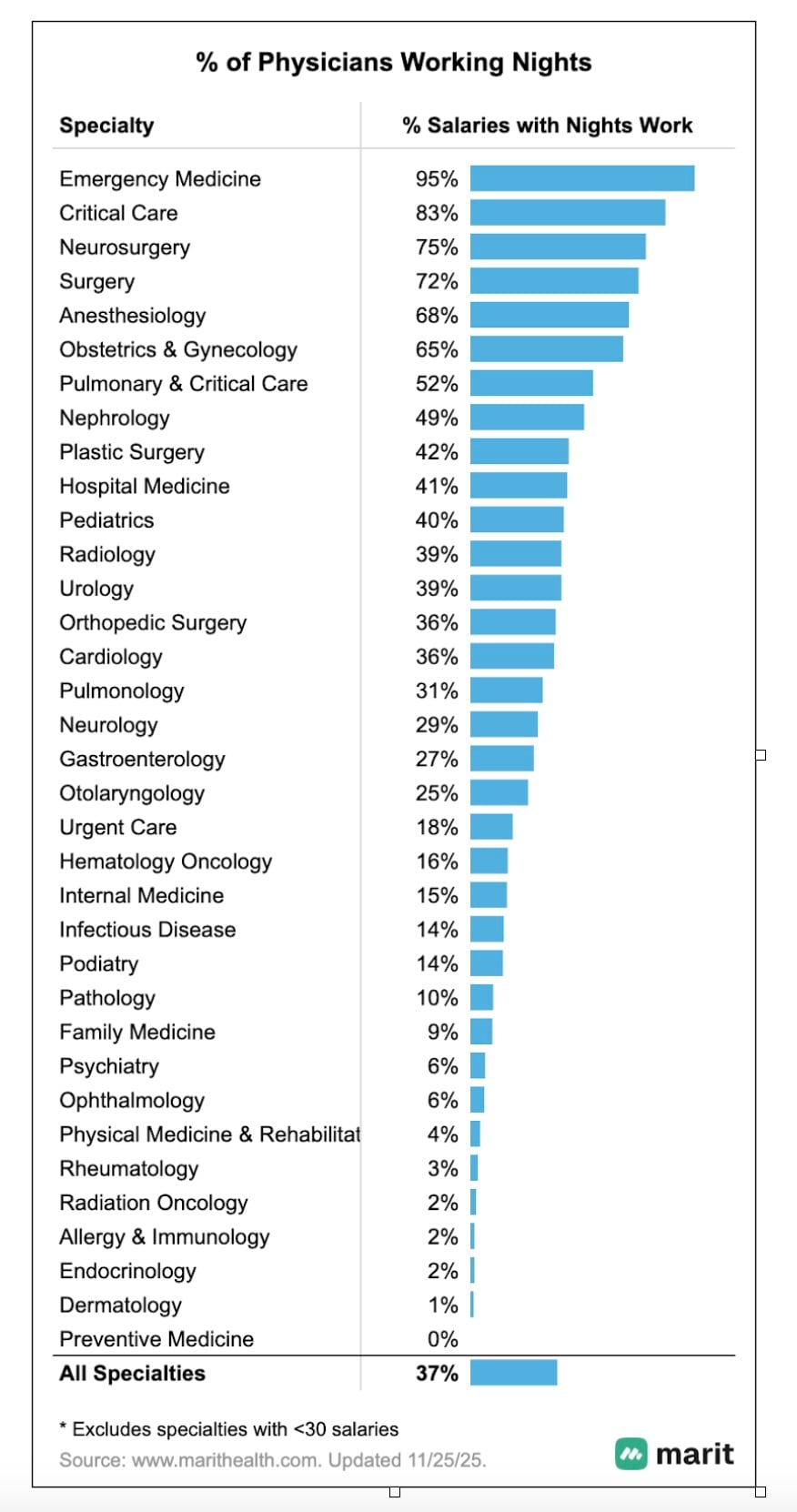
When we analyzed compensation patterns for night work among 20,000-plus anonymous salaries on Marit, one theme stood out: Night work is not the rare, career-stage-specific inconvenience many imagine them to be. More than a third of all physicians on Marit work at least some nights, and in some specialties, the expectation is nearly universal.
Unsurprisingly, emergency medicine tops the list, with 95 percent of physicians working nights. But they aren’t the only ones. In fields like critical care (83 percent) and surgery (72 percent), nights are the norm, not the exception. And even in specialties that don’t scream “overnight,” like pediatrics, urology, or orthopedic surgery, roughly one in three physicians still report working nights.
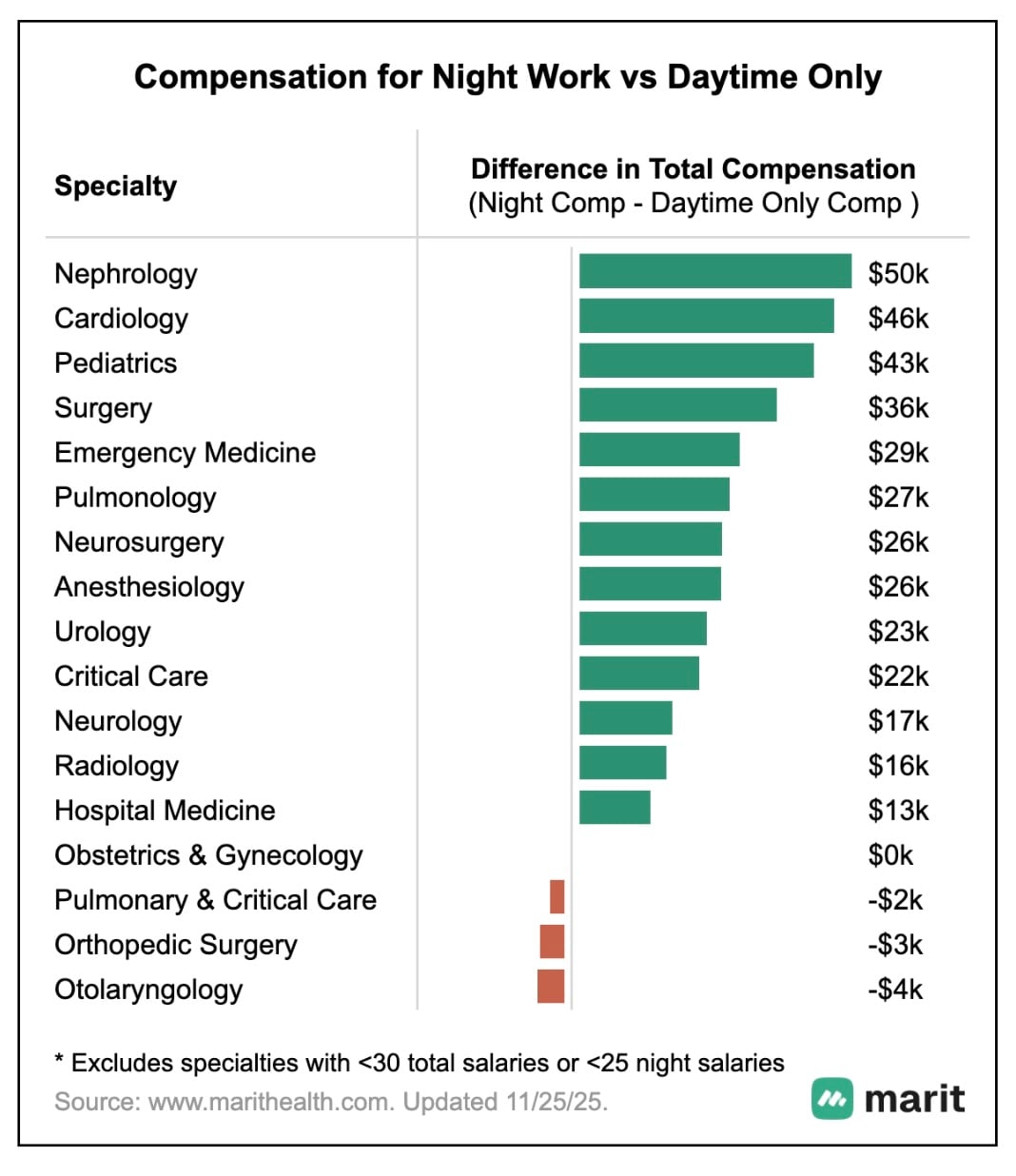
What’s even more interesting is that night work does not get rewarded evenly with higher compensation. When we compare salaries for clinicians who work nights against those who work day shifts only, the differences vary widely by specialty.
For some specialties, the night work premium is real and significant. Nephrologists earn about $50,000 more annually if they take night work compared to peers who work only days. Cardiology shows a $46,000 difference, followed by pediatrics at $43,000 and surgery at $36,000. Specialties like anesthesiology, urology, and critical care also see consistent differentials in the $22,000 to $26,000 range. The premium that comes with night work reflects a broader truth. Overnight work is both essential and hard to staff
But the pattern isn’t universal. In hospital medicine, the gap shrinks to just $13,000. In a few specialties like OB/GYN and orthopedic surgery, it disappears altogether. The reasons vary. In some cases, night coverage may be shared evenly across the group, without added compensation. In others, the differences may reflect the economic limits of night work itself; the pace and volume of overnight care rarely rival the productivity of daytime clinic or operative schedules, and compensation tends to mirror that.
My own nocturnist equation
That’s the macro view. But the personal financial impact for me was even more dramatic. I stepped away from leadership roles I had spent years building, and the stipend that came with them. I willingly left $50,000 on the table and still made more money on nights. Less responsibility. Less clinical load. More income. And then there’s the schedule: 26 weeks off per year. That time became the oxygen Marit Health needed to grow and the space for me to take care of myself for once. And if I ever wanted to ramp up and earn even more, I could take on extra shifts whenever I needed to. (I don’t, but I like having the option.)
On pure numbers alone, the financial upside and the time off created by night work were undeniable.
The psychological costs I didn’t expect
Here is the part I did not fully anticipate. The hospital at night is quieter, slower, and emptier. The usual rhythm of medicine disappears. There are fewer conversations, fewer co-workers around, and fewer moments of collaboration.
The isolation extends outside the hospital. When I am finally off and free, my friends and colleagues are busy with work or family. And when I am heading in for the night, they are settling into dinner or downtime with their families. The metaphor “ships passing in the night” feels very real. The separation becomes a part of daily life.
The lower clinical load also means fewer moments of clinical impact, the kind that remind you why you entered medicine. I have had to rethink how I measure meaningful work. It’s far less about production. It’s more about the small interactions with families surrounding a late-night trauma or the satisfaction of placing an epidural for an exhausted laboring patient. It also increasingly comes from building Marit, where I can help clinicians access real-world salary data and negotiate their contracts with confidence. Accepting that shift in identity took time.
Would I choose nights again?
Night float is a clear trade-off. The financial upside is undeniable. The schedule can afford you the flexibility and uninterrupted time to pursue other passions. But the costs are real as well, and would be too high for some. Night work reshapes your physiology in quiet ways. I feel healthier than ever in some respects, but I would be lying if I said I never think about the potential long-term health implications.
For where I am in life right now, the trade-off is worth it. I have more flexibility, more control, more time, more purpose, and yes, more income than I did before. I am using this window to build something that I hope will make decisions like this easier for the next generation of clinicians.
Rob Anderson is a practicing anesthesiologist and the physician co-founder of Marit Health, which is bringing salary transparency and a modern job board to medicine.





















![AI censorship threatens the lifeline of caregiver support [PODCAST]](https://kevinmd.com/wp-content/uploads/Design-2-190x100.jpg)
