For two months I have staged testimony, written op-eds, and amplified coalition voices about the collapse of developmental and behavioral pediatrics (DBP). This piece is an epilogue, a reckoning with a specialty that once held promise but now clings to aspirational posters instead of actionable reform.
The poster problem
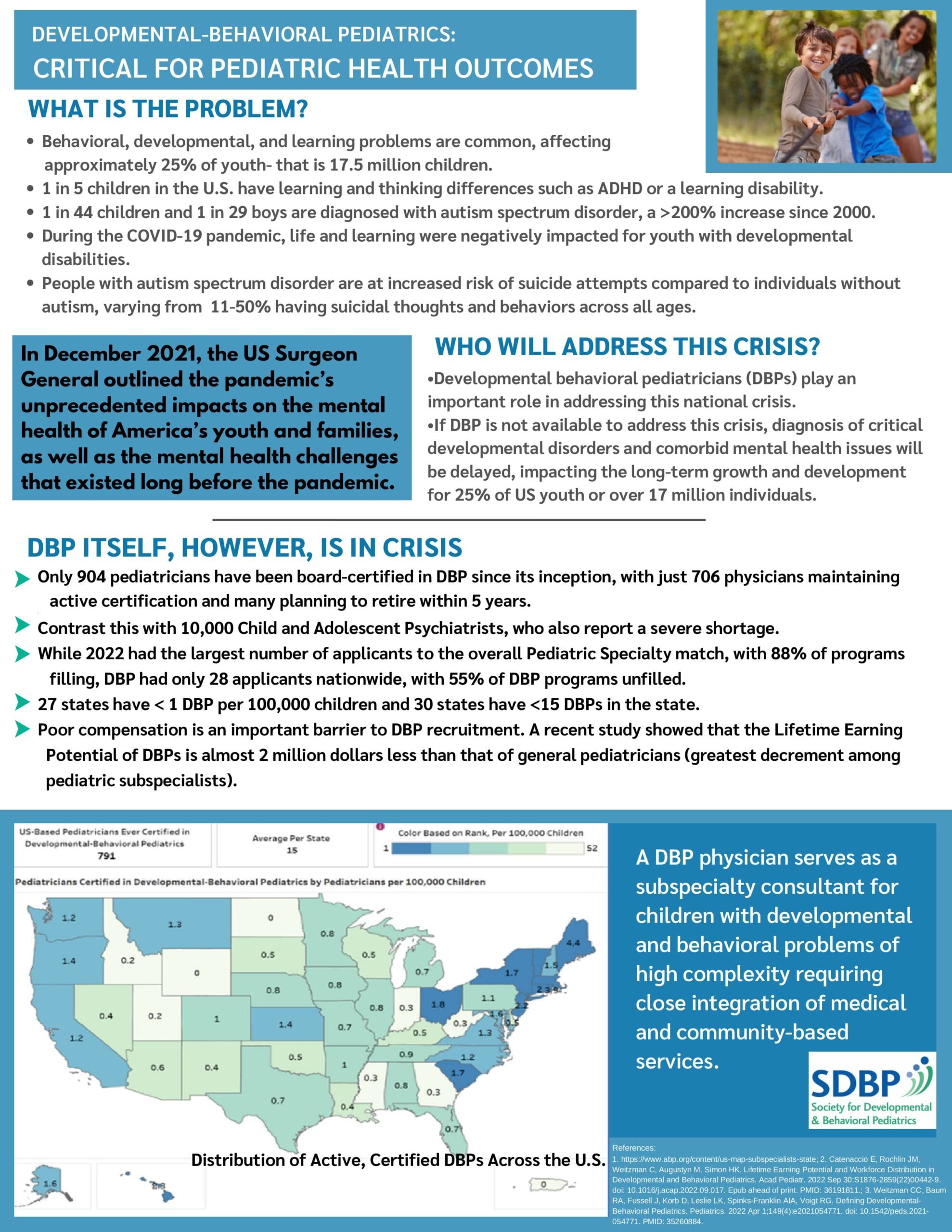
The Society for Developmental and Behavioral Pediatrics (SDBP) recently circulated a flyer titled Critical Outcomes in DBP. Page 2 lists “Solutions” to the recruitment crisis: recruit more BIPOC trainees, elevate DBPs into leadership, improve reimbursement, shorten fellowship training, expand telehealth parity, and increase research funding.
On paper, it looks hopeful. In reality, it is tone-deaf. These are slogans, not strategies. Posters, not pipelines.
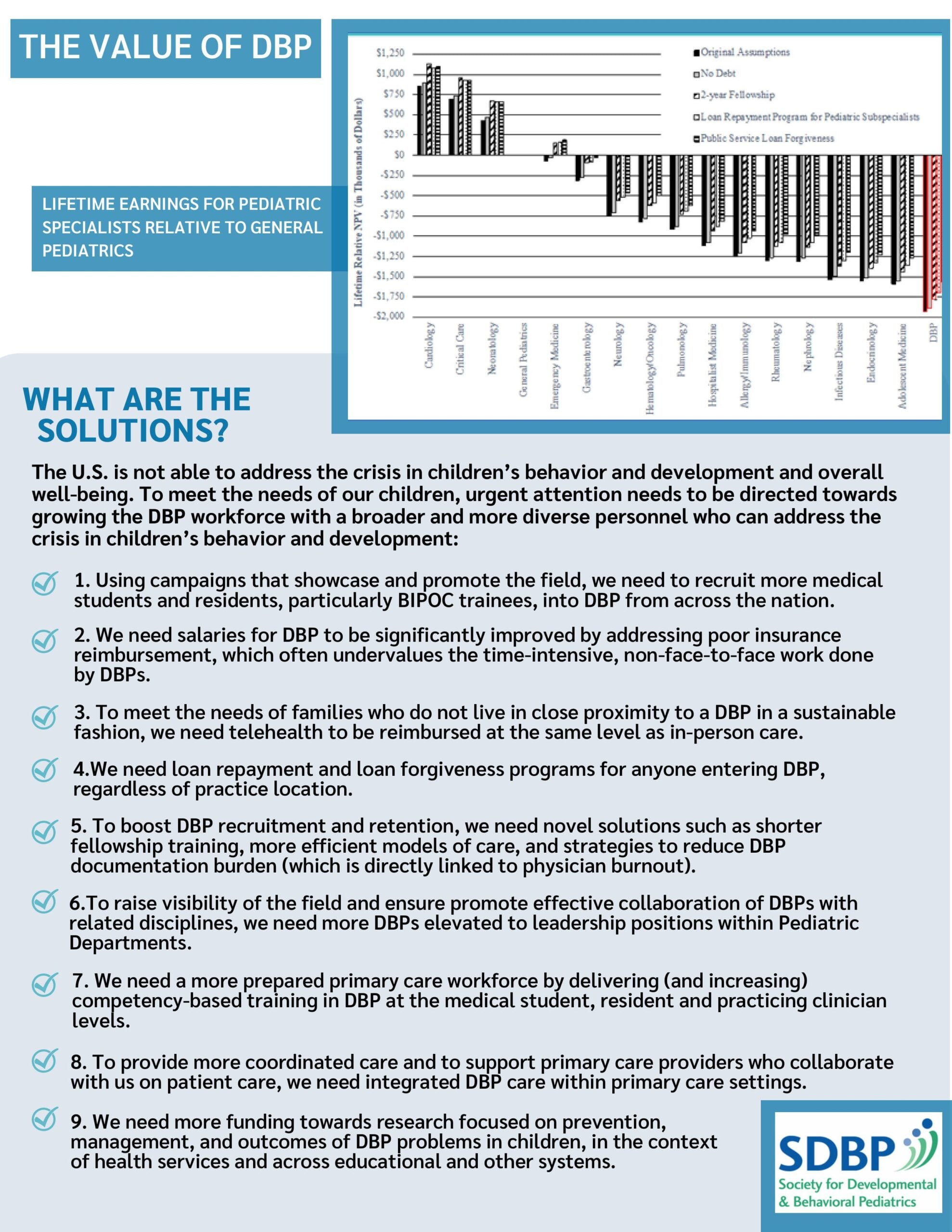
The flyer itself admits the truth: DBP has the lowest “lifetime relative net present value” (NPV) of any pediatric subspecialty, nearly $2 million less than general pediatrics. That is not just a statistic. It is a deterrent. Why would any graduate, especially one from a disadvantaged background, choose a disadvantaged field? Cardiology, critical care, and neurology offer higher pay, stronger prestige, and clearer pathways to leadership. DBP offers lower pay, higher burnout, and weaker institutional support.
That is why the flyer belongs in the text of this discussion, because it illustrates the gap between rhetoric and reality. It should not be tucked away as decoration. It is evidence.
Leadership without action
This collapse is not new. DBP once had a seat at the leadership table of the American Academy of Pediatrics (AAP). James M. Perrin, Judith S. Palfrey, and Benard P. Dreyer (all DBP physicians) served as AAP presidents. Their tenure could have been transformative. They could have addressed reimbursement inequities, pipeline fragility, and institutional invisibility. Instead, they did squat.
Leadership presence without leadership action is theater. It gave DBP visibility but no leverage.
I contrast this with leaders outside DBP (Toni Eaton, Howard Pearson, Joel Alpert) who were not DBP specialists but appreciated DBP issues. I knew them well, through training programs and the Children with Special Health Care Needs task force. They understood the stakes. They respected the field. Yet even their advocacy could not overcome the inertia of a specialty unwilling to fight for itself.
My own path
I completed a two-year DBP fellowship. But before that, I had four years of practical experience in the United States Air Force. That frontline training gave me operational clarity: DBP needed structural fixes, not slogans.
When I applied for a LEND program, I did not submit a poster. I submitted an actionable plan: funded, interdisciplinary, measurable. LEND programs work because they are structured, resourced, and accountable. They recruit trainees by offering real incentives, not aspirational rhetoric.
That is the difference between action and aspiration. Between command and theater.
The pipeline illusion
In 2022, only 28 applicants nationwide applied to DBP fellowships. More than half of programs went unfilled. That is not a pipeline; it is a drip. Posters will not fix that. Loan forgiveness might. Reimbursement parity might. Funded interdisciplinary programs like LEND certainly will.
But slogans alone will not.
The SDBP flyer’s “solutions” are tone-deaf because they ignore the economics. They ask BIPOC graduates (often carrying heavier debt loads) to enter a field with the worst financial outlook in pediatrics. That is not equity. That is exploitation disguised as diversity.
Why I stayed, why I still speak
I did not enter this field to get rich. I entered because I had both a calling to do something, and the gifts to get it done. For years, I carried that calling through fellowship, through service in the Air Force, and through practice. Eventually, I burned out and took early retirement.
I am comfortably settled now because I was prudent with money. But I never left the arena. I remain in the arena still, even as my body cannot keep pace with my mind in advocacy.
That is why I write. That is why I speak. Because DBP deserves better than posters. Families deserve better than slogans. Children deserve better than tone-deaf leadership.
And because when history records this era, it should not say that DBP collapsed without witness. It should say that some of us remained in the arena, calling for action when others settled for aspiration and inaction. I shall remain in the arena as long as my body and the good Lord allow me to bear witness.
Ronald L. Lindsay is a retired developmental-behavioral pediatrician whose career spanned military service, academic leadership, and public health reform. His professional trajectory, detailed on LinkedIn, reflects a lifelong commitment to advancing neurodevelopmental science and equitable systems of care.
Dr. Lindsay’s research has appeared in leading journals, including The New England Journal of Medicine, The American Journal of Psychiatry, Archives of General Psychiatry, The Journal of Child and Adolescent Psychopharmacology, and Clinical Pediatrics. His NIH-funded work with the Research Units on Pediatric Psychopharmacology (RUPP) Network helped define evidence-based approaches to autism and related developmental disorders.
As medical director of the Nisonger Center at The Ohio State University, he led the Leadership Education in Neurodevelopmental and Related Disabilities (LEND) Program, training future leaders in interdisciplinary care. His Ohio Rural DBP Clinic Initiative earned national recognition for expanding access in underserved counties, and at Madigan Army Medical Center, he founded Joint Base Lewis-McChord (JBLM) CARES, a $10 million autism resource center for military families.
Dr. Lindsay’s scholarship, profiled on ResearchGate and Doximity, extends across seventeen peer-reviewed articles, eleven book chapters, and forty-five invited lectures, as well as contributions to major academic publishers such as Oxford University Press and McGraw-Hill. His memoir-in-progress, The Quiet Architect, threads testimony, resistance, and civic duty into a reckoning with systems retreat.



















![AI censorship threatens the lifeline of caregiver support [PODCAST]](https://kevinmd.com/wp-content/uploads/Design-2-190x100.jpg)
