An excerpt from The Parkinson’s Plan: A New Path to Prevention and Treatment.
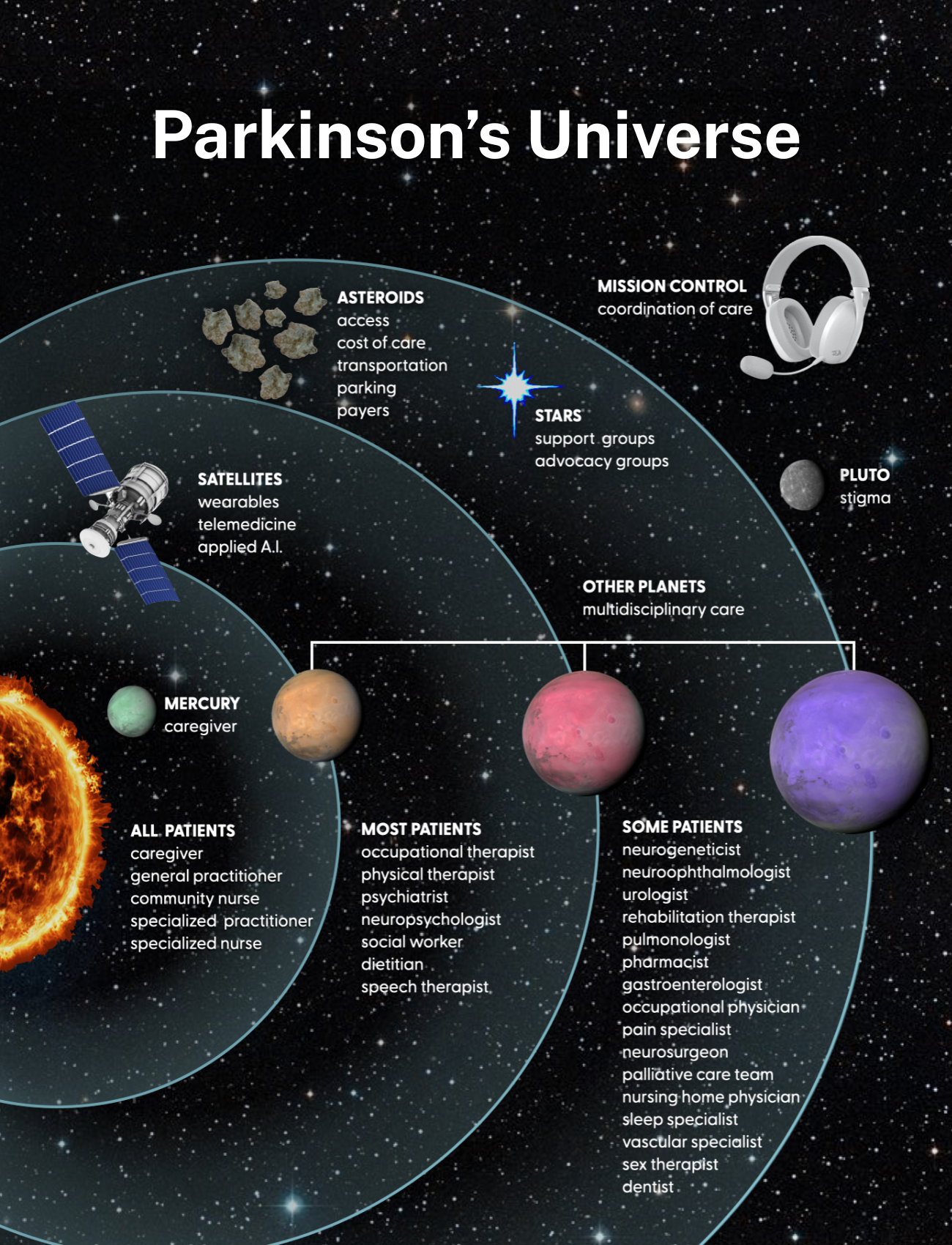
The Parkinson’s universe
In 2002, we proposed a simple Parkinson’s care model. The patient is the sun, and all multidisciplinary care should orbit around the patient, not the doctors. The sun is vital but only part of the universe. It is time to expand our Parkinson’s care model.
The caregivers
If we stick to the universe analogy, caregivers are represented by the planet Mercury. Mercury is the closest planet to the sun, and though the smallest in the solar system, it is vitally important. It is fitting for the caregivers to be represented by Mercury as the name represents the Roman god of commerce and communication. Mercury (the caregiver) is the messenger to the patient (the sun) and to the rest of the universe. Mercury is heavily cratered on its surface, due to the impact of many collisions. Caregivers must absorb the many challenges of living with a person with Parkinson’s, and there are frequently long periods of darkness and light. Mercury (the caregiver) has the closest connection to the sun (the patient), and the planet can get hot.
Multidisciplinary specialists
The sun’s (patient’s) gravity holds the solar system together. The connections and interactions drive the seasons, ocean currents, weather, and climate. In our model, the other planets beyond Mercury (the caregiver) represent the many multidisciplinary specialists who are attracted by the gravity of the sun (the patient) and who all stay in orbit to provide necessary elements of Parkinson’s care.
Access and stigma
There are many challenges to the optimal care of Parkinson’s. We refer to these challenges in the Parkinson’s Universe as asteroids. Asteroids are dangerous rocks or metals that are too small to be planets but also orbit the sun.
Some astronomers believe they are leftover, building materials from planets that were not completely formed. They can be boulder to city sized, and one, named Ceres, has been referred to as a dwarf planet due to its small size (just 940 kilometers in diameter). In the Parkinson’s Universe patients must avoid asteroids, which include access to and distance from care, parking, and stigma. Finally, the darker side of the universe, filled with treacherous asteroid fields, is the insurance companies.
New technologies to link care
Modern care plans for Parkinson’s disease would not be complete without exploiting the benefits of technology. We envision the technologies as orbiting satellites, which can be accessed anytime and anywhere by the person with Parkinson’s or their caregiver. These include telemedicine, wearable devices like Fitbits and Apple watches, and artificial intelligence (AI).
Mission control and care coordination
At NASA, mission control is a team responsible for overseeing and managing complex operations. Most people identify mission control with space exploration; however, the term can be applied to operations. In the Parkinson’s Universe, patients and family members need a center of operations. We consider mission control to be vital especially when launching (new medications or therapies), orbiting (maintaining programs such as exercise, diet, and healthy living), and reentering the atmosphere (socially reintegrating into society and facing stigma). For space, mission control includes technical specialists, flight directors, engineers, and communication officers.
Support and advocacy groups
The final piece in the Parkinson’s Universe includes all the voices, the support networks, and the families navigating the disease. We see these support groups, networks, and advocacy organizations as the many stars in the sky. A person or family can look up at any time and find a light for their path.
The patient is the sun.
There are so many ways to reimagine caring for individuals with Parkinson’s. The modern American health care system has been built on a primary care “gatekeeper” model. You are required to select a primary care doctor who effectively controls your care. When a medical problem escalates beyond the gatekeeper’s expertise, they send a request on your behalf for evaluation by an appropriate specialist. The gatekeeper system presents a myriad of challenges for Parkinson’s patients. First, there may or may not be a specialist in the network covered by the person’s insurance. Second, if there is one, the wait time is often months. Third, the specialist may have little or no experience managing Parkinson’s disease as it relates to their specialty. Fourth, there is usually little or no multidisciplinary discussion among the clinicians.
There are four core principles to pull off implementation of a hub-based model of care for Parkinson’s disease.
All interdisciplinary specialists who will be required to provide optimal care are colocated under one roof. In the case of Parkinson’s disease and other movement disorders, for example, neurology, neurosurgery, neuropsychology, psychiatry, physical therapy, occupational therapy, speech/swallow therapy, and social workers all evaluate patients at a common facility. Patients can be prescheduled with multiple specialists or scheduled on demand, and practitioners can interact in real time, especially if warranted by the complexity of the case.
We hear everyone’s voices. Each specialist develops and communicates a patient-specific care plan within their area of expertise, and follow-up can be accomplished in the local community if the patient lives remotely. Documentation of all subspecialty evaluations and recommendations is sent to referring care providers and any other designated local care provider, is shared directly with each patient, and can be reviewed via the online medical record system.
Every patient is a potential research participant, and outcomes of all therapeutic interventions are carefully documented and tracked over time. Each patient signs an institutional-review-board-approved database consent, so that every contact with a patient becomes part of both the clinical record and the research database. Patients also specify whether they are willing to be contacted for potential inclusion in future research studies. An effort is undertaken by all specialists to perform consistent structured evaluations at regular intervals in order to maximize the uniformity of clinical data. Clinical research trials are available and conducted in the same facility.
The relationship between the patient and each of the care or research providers is bidirectional. Interactions are not solely for the patient’s benefit. The hub focuses on the professional and personal needs of each provider, as well as the needs of each patient. Bidirectionality facilitates research to improve care, enhances the education of the next generation of specialists, and fosters professional development and workplace satisfaction.
We continue to deliver a new diagnosis every six minutes, and the Parkinson’s population is on track to more than double by 2040. Millions hope for a cure; yet we meander in our efforts to care for them. It is time we improve our command and control for Parkinson’s.
Ray Dorsey and Michael Okun are neurologists and authors of The Parkinson’s Plan: A New Path to Prevention and Treatment.



















![Stopping medication requires as much skill as starting it [PODCAST]](https://kevinmd.com/wp-content/uploads/The-Podcast-by-KevinMD-WideScreen-3000-px-4-190x100.jpg)
![Weaponizing food allergies in entertainment endangers lives [PODCAST]](https://kevinmd.com/wp-content/uploads/The-Podcast-by-KevinMD-WideScreen-3000-px-3-190x100.jpg)


![AI censorship threatens the lifeline of caregiver support [PODCAST]](https://kevinmd.com/wp-content/uploads/Design-2-190x100.jpg)
